THE FUTURE OF WORK IN HEALTHCARE IS HERE
In technological terms, the future is already here. But in many provider organizations, the plan for working in that future is still on the drawing board. Organizations have the opportunity to fuse talent and technology or to have them “join forces” instead of burdening or competing with one another. To do so they need to intentionally coordinate human and technological resources from the outset.
The nature of work across almost every industry is being disrupted by a number of factors. Rapidly evolving digital technology is driving increased automation, affecting the proximity of where work is performed, and giving rise to new operational models that enable talented people to perform better. With so much change in the air, many provider organizations are understandably apprehensive about how to grapple with such exponential change and its implications on how, where, and by whom work gets done. What these organizations need to keep in mind with this shift is the immense opportunity to alleviate current pain points like nursing shortages and physician burnout, and refocus professions on mission-oriented, fulfilling work.
World Economic Forum founder, Klaus Schwab, has dubbed this transformation in the way work as “the Fourth Industrial Revolution”, making the distinction that it is not about replacing people, but rather how new technologies are “fusing the physical, digital, and biological worlds”. This augmented workforce combines people and machines to get things done in a way that is not only more productive, but also more rewarding for the worker.
Interestingly, while 69 percent of US health care providers consider the augmented workforce to be an important trend, only 33 percent feel the same way about robotics, cognitive computing, and artificial intelligence. What these providers may not appreciate is that all these areas are part of the same wave of change.
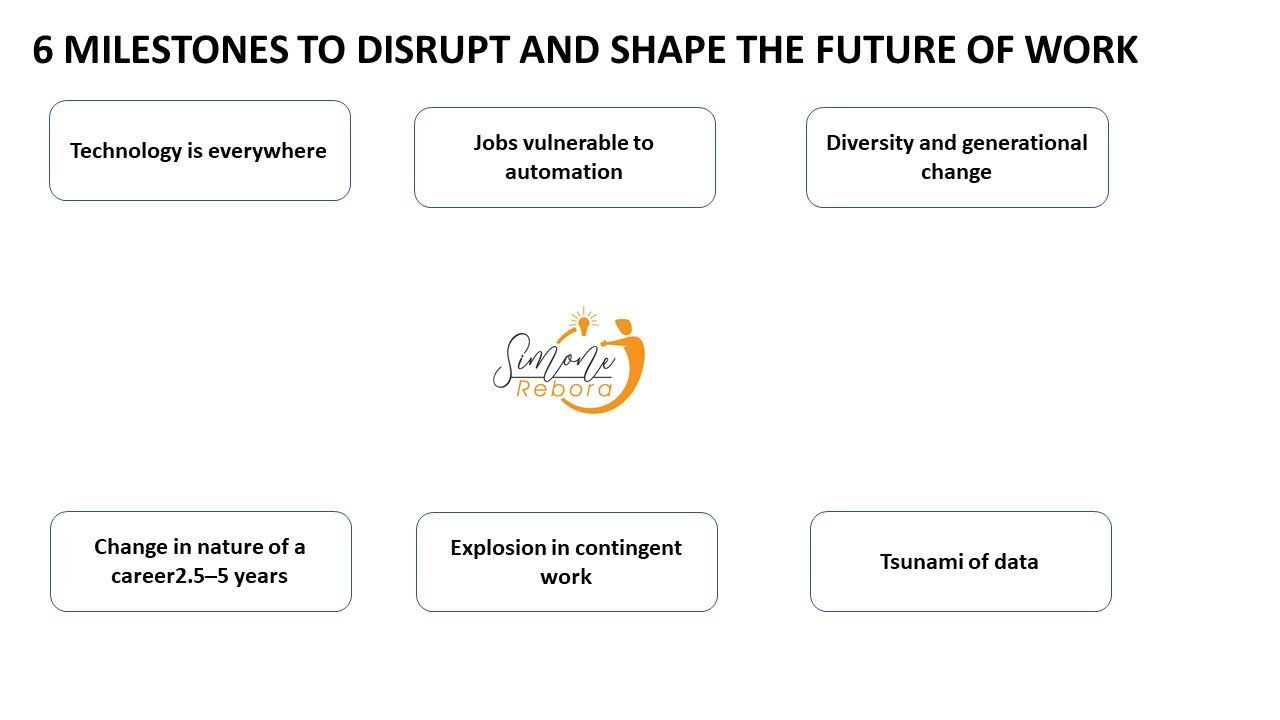
Seven disruptors shape the future of work (source Deloitte article):
1) Technology is everywhere, 6 billion+ smartphones in the world by 2020
2) Cognitive computing, robotics affordability, $500,000 in 2008, $22,000 in 2020
3) Jobs vulnerable to automation 35% UK 47% US 77% China
4) Diversity and generational change, Millennials reaching 50% of workforce
5) Change in nature of a career 2.5–5 years: Half-life of skills
6) Explosion in casual work US casual workers 40% by 2020
7) Tsunami of data 9X more in last 2 years
Organizations have the opportunity to fuse talent and technology or to have them “join forces” instead of burdening or competing with one another. To do so they need to intentionally coordinate human and technological resources from the outset. The organizations that fail to do so risk missing out on great leaps in efficiency and engagement. From a health care perspective, it can mean a demotivated workforce with growing nursing shortages and high levels of burnout, a reduced ability to attract and retain highly skilled clinicians and non-clinicians, a reduction in the quality of care, and a loss of position as a patient’s provider of choice.
THE FUTURE OF WORK IN HEALTHCARE
Plenty of technology. Rapid change. Workforce uncertainty. And no shortage of well-entrenched “ways we’ve always done things.” Few industries match this description better than health care. Although 100% of health care providers surveyed in the 2017 Deloitte Human Capital Trends report plan to make significant progress in adopting cognitive and artificial intelligence (AI) technologies in the next three to five years, and 33% say they consider it a priority to train employees so they can work side by side with robots and AI, however none have made significant progress in adopting these technologies. One reason for this may be that many leaders of health care provider organizations anticipate that the scale and pace of change will overwhelm their workforce and compound current challenges, such as a short supply of nurses and a burned-out physician population. What these executives may not be considering is that these shifts – and subsequent disruption to the automation of tasks, proximity of where work is performed, and evolution of new and open talent models – represent a tremendous opportunity to help resolve those current challenges. Today’s hospital systems are asking, “How can we hire and retain more nurses to combat our labor shortage?” The question they should ask instead is, “How can we augment nursing roles so that high-performing nurses wouldn’t want to work anywhere else?” To answer this question, provider organizations will need to assess the trajectory of specific jobs and workflows, evaluating the mix of factors that combine to operate those jobs and workflows and how they can be re-envisioned by employing enabling technologies and new talent models:
- Talent category: Is this a full-time, in-house job? To what extent can different categories such as contract, off-balance-sheet, or crowdsourcing, accomplish this?
- Automation level: How much of the work is made up of tasks that can be delivered through either physical robotics, cognitive automation, or a combination? What skill-based parts of the job must remain in human hands?
- Physical proximity: Must this job be performed in person? Does the practitioner need to be present at the site of service delivery? What about the patient?
In technological terms, the future is already here. But in many provider organizations, the plan for working in that future is still on the drawing board. As each provider organization seeks to map out its own workforce strategy, it needs to adopt an exponential mindset: Each part of the workforce will evolve not along a single linear path, but in response to a collection of forces. Rather than fearing this wave of change as an overwhelming challenge, provider organizations should proactively seek out the opportunities for augmentation and automation in clinical workflows – and pinpoint where both clinicians and patients will benefit from new technologies, innovative talent models, and expanded locations where care is delivered.



